Human Papillomavirus (HPV) and Cervical Cancer
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection of the reproductive tract. Most sexually active men and women will be infected at some point in their lives, and some may be repeatedly affected (World Health Organization, 2020). In both men and women, the peak time for acquiring the infection is usually shortly after becoming sexually active. Penetrative sex is not a requirement for transmission of this sexually transmitted virus. Skin-to-skin genital contact is a regular mode of transmission.
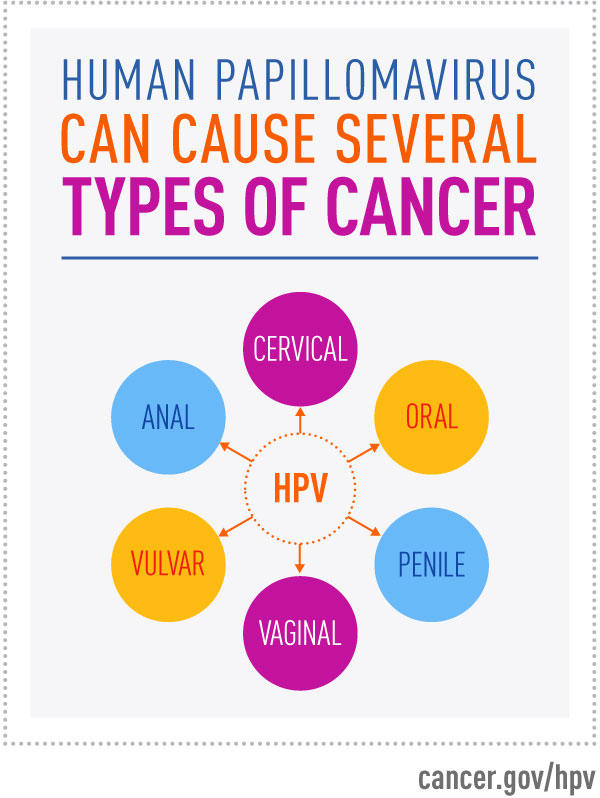
HPV is of many strains, and most do not cause problems. The infection usually disappears within a few months after the acquisition, and about 90% clear within two years. However, certain types of HPV can persist and progress to cervical cancer. The most common HPV-related disease is cervical cancer. Almost all cases of cervical cancer are the result of HPV infection. Certain strains of HPV can also cause cancer of the anus, vagina, vulva, penis, and oropharynx (World Health Organization, 2020).
Non-cancer causing types of HPV can cause genital warts and tumor growth in the airway passage from the mouth and nose into the lungs.
Almost all HPV infections clear up on their own, and most pre-cancerous lesions resolve spontaneously. Still, the risk exists that HPV infection may become chronic, and pre-cancerous lesions may progress to invasive cervical cancer. In women with a healthy immune system, it usually takes 15 to 20 years for cervical cancer to develop. However, it can take only 5 to 10 years in women with weakened immune systems, such as untreated HIV infection (World Health Organization, 2020).
Cervical Cancer Intervention and Prevention
- Community education
- Social mobilization
- Vaccination Screening
- Treatment and palliative care
- Vaccination for girls 9-14 years
- Health information and warnings about tobacco use
- Male circumcision
- Sex education tailored to age and culture
- Surgery
- Chemotherapy
- Radiotherapy
- cryotherapy
- Condom promotion and provision for those engaged in sexual activity
- Palliative care
- Screen sexually active women for abnormal cervical cells and pre-cancerous lesions, starting from 30 years of age (World Health Organization, 2020).
References
World Health Organization. (2020). Human papillomavirus (HPV) and cervical cancer. Retrieved from:
https://www.who.int/news-room/fact-sheets/detail/human-papillomavirus-(hpv)-and-cervical-cancer
Comments
Post a Comment